Background: According to the Iodine Global Network, the Russian Federation is a region of mild iodine deficiency. At present, in Russia there is no systematic monitoring of the state of iodine deficiency in the regions. Existing legislation establishes the voluntary nature of iodine prophylaxis. In this regard, the issue of studying the iodine supply of the population of the Siberian region on the example of the city of Novosibirsk is relevant.
Aim: of research is to evaluate the availability of iodine and the effectiveness of the prevention of iodine deficiency among teenagers 13-18 years old and young people 19-25 years old in Novosibirsk.
Materials and methods: The research includes representative samples of pupils from 13 to 18 years old (612 people of both sexes, 62 of them have completed a questionnaire about the use of iodized salt, urine samples do determine UIC were taken from 60 of them ) and young people from 19 to 25 years old (101 people of both sexes. They all filled out the proposed questionnaire, 27 people were identified UIC). We used such methods as questionnaires, determination of UIC, comparison of the obtained data with the results of clinical and population studies conducted in Novosibirsk in 1994-1995, 2004-2005, 2009-2010.
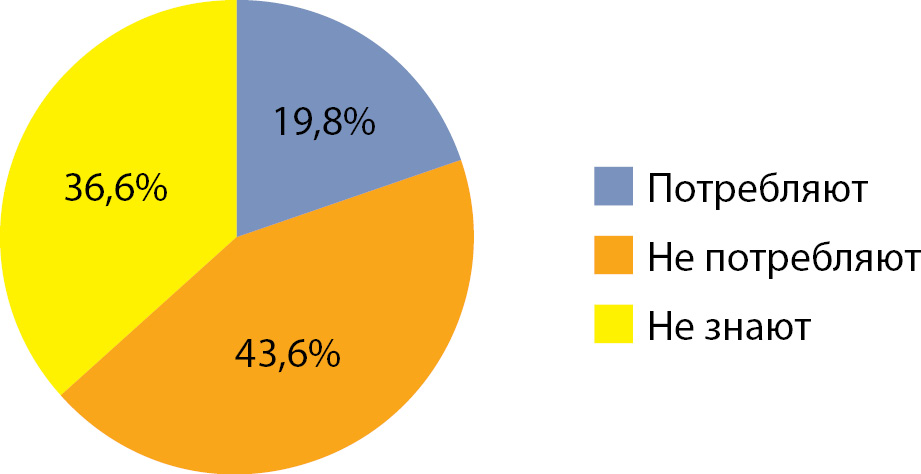
Results: In 2005 32.7% of adult population consumed iodized salt. In 2010, 47% of adolescence surveyed consumed iodized salt. According to a survey conducted in 2019 it was found that among adults 19-25 years old 19.8% know that they consume iodized salt. Among schoolchildren from 13 to 18 years old, 8.1% know for sure that use iodized salt. In 1994-1995 mUIC in persons of reproductive age in Novosibirsk was 47 μg / L. In 2005 mUIC in the adult population (45-69 years old) was 107 μg / L. In 2010 mUIC was 93 μg / L, UIC less than 50 μg / L was determined in 7% of samples, among school children. In 2019 MUIC amounted to 111 μg / l in adult population, the proportion of urine samples with UIC less than 50 μg / l - 10.7%. MUIC was 123 μg / l in 2019 among adolescence, the proportion of urine samples with UIC less than 50 μg / l - 14.5%.
Conclusions: Over the 24-year period of observation, there is a significant improving the iodine supply of the population in Novosibirsk. The low awareness of the young generation of the inhabitants of Novosibirsk about iodine deficiency and measures for its prevention was recorded.