Original Studies
Thyroid hormone deficiency negatively affects the state of the cardiovascular system, causing the formation of a «myxedematous heart». The frequency and clinical features of primary hypothyroidism in 84 patients discharged from the endocrinology department of the RCH in 2017-2022 were retrospectively analyzed. Pericardial effusion was registered in 9 people (10.7%). Massive effusion with separation of pericardial leaflets from 30 to 50 mm and the threat of tamponade was in 4 out of 9 patients. Even with a large volume of pericardial effusion, classic symptoms such as shortness of breath, orthopnea, chest pain, and a feeling of fullness were absent or poorly expressed. Differential diagnosis with diseases accompanied by accumulation of fluid in the pericardial cavity was required. Indicators of thyroid status made it possible to associate the hydropericardium with decompensation or hypothyroidism for the first time. Thyroid hormone replacement therapy led to the disappearance of hypothyroidism symptoms and a decrease in the hydropericardium. With a high risk of tamponade in 3 patients, therapy was supplemented with pericardiocentesis. A clinical observation of successful treatment with thyroid hormones in combination with pericardiocentesis of severe newly diagnosed hypothyroidism against the background of autoimmune thyroiditis with massive pericardial effusion is presented.
BACKGROUND: Congenital subclinical hypothyroidism is a condition made when a serum TSH is elevated with circulating thyroid hormone levels within their reference ranges, revealed as a result of neonatal screening. To date, the question of the effect of this condition on the physical and neuropsychic development of children remains open, in addition, there are no clear indications for the choice of therapeutic tactics and the start of substitution therapy.
AIM: To evaluate the impact of therapeutic approaches on the neuropsychiatric and physical development of children with congenital subclinical hypothyroidism.
MATERIALS AND METHODS: A statistical analysis of thyroid profile, physical and neuropsychiatric development indicators was carried out between two groups of patients with congenital subclinical hypothyroidism, depending on the therapy received.
RESULTS: There was a statistically significant decrease in TSH compared with the baseline, as well as maintaining the initially normal level of free thyroxine in the group of patients receiving hormone replacement therapy, after re-testing and discontinuation of therapy. None of the patients included in the study were diagnosed with the development of manifest hypothyroidism during dynamic follow-up. There were no statistically significant differences in hight, target hight, BMI, neuro-psychiatric development between two groups.
CONCLUSION: The first evidence was obtained of the absence of the effect of «elevated» TSH levels on the neuropsychological and physical development of children with congenital subclinical hypothyroidism during dynamic observation (at least the first 4 years of life), which gives the clinician additional arguments when discussing the choice of therapeutic tactics for congenital subclinical hypothyroidism.
OBJECTIVES: Congenital hypothyroidism (CH) is one of the common thyroid disorders in children. Early detection and prompt initiation of hormone replacement therapy (HRT) are important for further normal neonatal development. In clinical practice, one of the key problems is the differentiation of fT4 level to identify cases of obvious hypothyroidism requiring immediate prescription of levothyroxine, and subclinical hypothyroidism, allowing the clinician to understand the causes of elevated TSH during dynamic monitoring and make a cardinal decision on the need for lifelong HRT.
AIM: To establish the values of the lower limit of the reference interval (LLRI) for fT4 in newborns to decide on therapeutic tactics.
MATERIALS AND METHODS: Until 2013 laboratory tests were performed on a «Wallac DELFIA» analyser (normative values for fT4 9.8–16.8 pmol/l), then on a «bioMerieux VIDAS» analyser (normative values for fT4 10.6–19.4 pmol/l). RI was determined based on the results of cT4 measurements in newborns examined in the neonatal screening framework at the clarifying diagnosis stage.
RESULTS: LLRI for fT4 of all 1596 neonates was 10.9 pmol/l (90% CI 10.5; 11.1), in full term neonates — 11.10 pmol/l, (90% CI 10.70–11.60 pmol/l); in premature neonates — 9.63 pmol/l (90% CI 9.20–11.30 pmol/l).
ONCLUSIONS: in clinical practice, it is reasonable to use the cut-off point for fT4 below 11.0 pmol/l to decide on the need for HRT, irrespective of the day of clarifying diagnosis and gestational age. If the level of fT4 is higher than 11.0 pmol/l, regardless of the level of TSH increase, it is possible to interpret this condition as subclinical hypothyroidism and to choose the tactics of dynamic follow-up with monthly control of thyroid tests.
BACKGROUND: Graves’ disease (GD) is a common cause of persistent thyrotoxicosis. In regions with adequate iodine intake, the incidence is 20–30 cases per 100,000 people. Modern treatment of GD includes antithyroid drugs, radioactive iodine therapy (RAI), and thyroidectomy. The choice of treatment strategy is based on the severity of thyrotoxicosis, the frequency of potential side effects, the availability of treatment options, and the likelihood of achieving sustained remission. Previous studies have demonstrated differences in approaches to diagnosis, treatment, and follow-up between countries and individual specialists.
AIM: To conduct a survey on the current clinical practice of treating Graves’ disease in Russia.
MATERIALS AND METHODS: An online survey was conducted among physicians in 2022-2023. The questions covered the principles of diagnosis, treatment, and dynamic observation of adult patients with Graves’ disease.
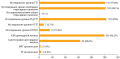
RESULTS: The study involved 104 physicians of various specialties who treat patients with Graves’ disease. Approximately 99% of respondents chose the determination of thyroid-stimulating hormone receptor antibodies (TSHR-ab) to clarify the etiology of thyrotoxicosis, while only 60.6% of them chose thyroid scintigraphy. As the first-line treatment method, antithyroid drug therapy is chosen by 88.5%, while 13.5% of physicians use radioactive iodine therapy (RAI), and less than 1% of respondents refer patients to thyroidectomy. Thiamazole is most commonly used (99%), while propylthiouracil (PTU) is used in cases of allergy to thiamazole or during the first trimester of pregnancy. The «block-replace» scheme is preferred over the «block» scheme, with 72.1% compared to 28.8%, respectively. The majority of physicians (95.2%) initiate therapy with moderate doses of thiamazole (20–30 mg) and PTU (200–300 mg). Most physicians conduct dynamic monitoring of liver transaminase levels (57.7%) and complete blood count (78.8%). Conservative therapy is prescribed for a period of 12–18 months (88.5%) or up to 24 months (10.6%). Before discontinuing antithyroid drug therapy, 89.4% of respondents monitor thyroid hormone levels, 82.7% monitor TSHR-Ab levels, and 47.1% perform thyroid ultrasound. Repeat courses of conservative therapy are prescribed for up to 61.5% of respondents. Approximately 63.5% of surveyed physicians reported difficulties in referring patients for radical treatment due to a limited number of specialized institutions. Physicians cited patient unwillingness and the need to postpone pregnancy (81.6% and 24.3% respectively) as the main inhibitory factors for RAI. Thyroidectomy was associated with patient unwillingness (69.2%), as well as physician fear of laryngeal paralysis (48.1%) and postoperative hypoparathyroidism (49%).
CONCLUSION: The results of the study demonstrated that physicians in their practice generally adhere to international recommendations for the treatment of Graves’ disease.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2310-3787 (Online)